Eliminating humidity issues in sterile hospital storage areas

- Home
- Insights
- Humidity control and drying insights
- Eliminating humidity issues in sterile hospital storage areas
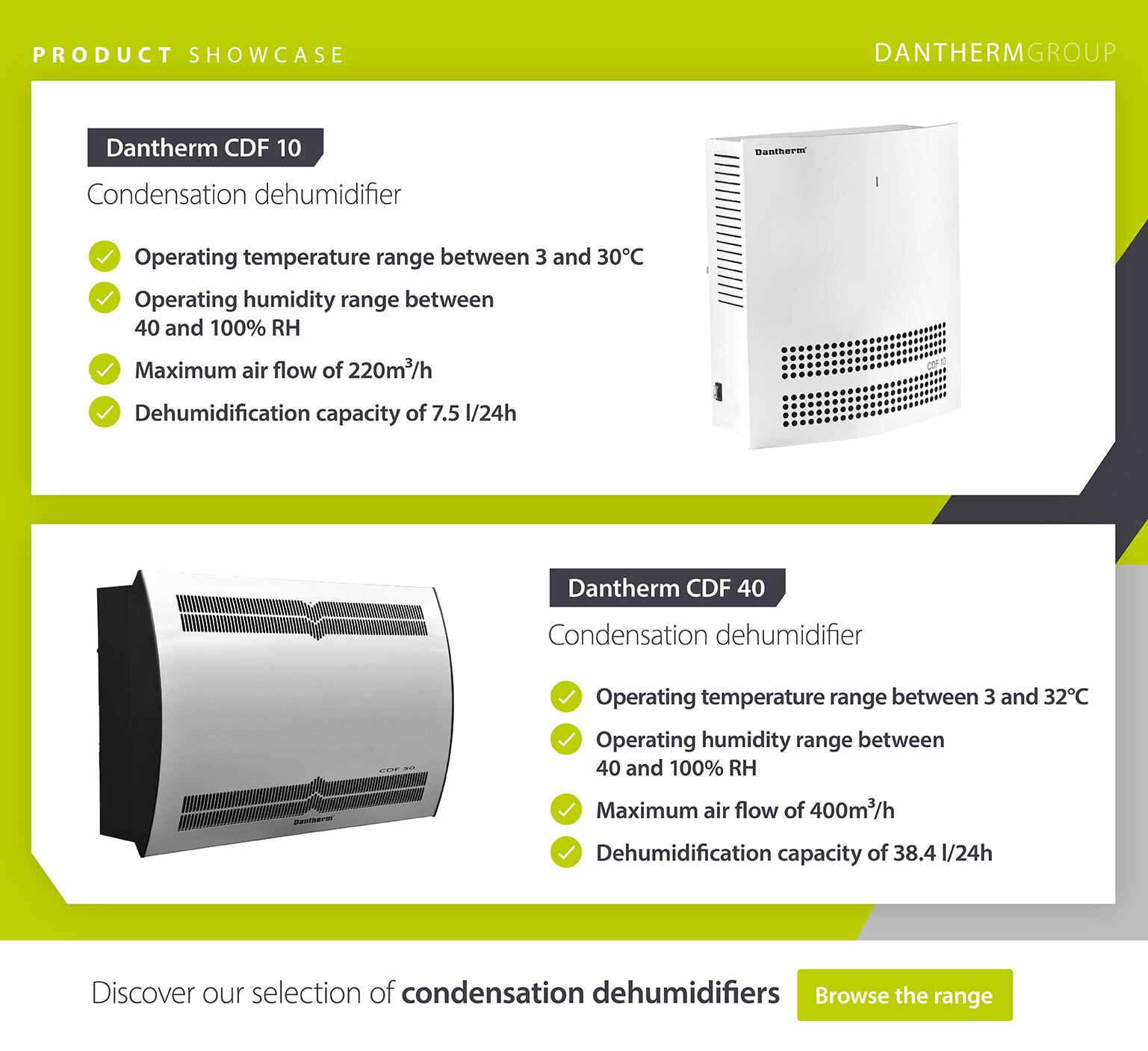
High humidity, especially during the summer, is known to cause problems related to growth of microorganisms in storage areas for sterile equipment and materials at hospitals. A recent university degree project study carried out by Susan Johansson, a master’s student at the University of Skövde, has demonstrated that Dantherm’s CDF 10 and CDF 40 condensation dehumidifiers can keep the air quality within national recommendations without increasing the risk of microbial growth in a very cost-effective manner. Here’s the story.
High humidity in hospital storage rooms – a health risk to patients?
High humidity, especially in the summer, has long been a problem in surgical units around Sweden. This had led to postponements and even cancellations of planned surgery, which in itself poses a potential health risk to some patients. Sterile equipment has also had to be discarded or re-sterilised due to contamination when moisture has entered the packaging. This is very costly and time-consuming but necessary to ensure that sterile purity is maintained. Sterile purity means that a maximum of one living micro-organism can be present in one million instruments. Sterile purity is the criterion for skin and/or mucous membrane penetration. Sterile material should be kept sterile until use on a patient.
In terms of patient safety, the problems that high humidity can generate in a surgical environment with high humidity over time is that sterile material risks being contaminated by microbial growth. It can then be brought into the operating theatre and contaminate the sterile field and pose a risk to the patient, for instance causing postoperative wound infections. Postoperative wound infections are one of the most common healthcare- associated infections in Sweden and cause a total of about 20% of them. Postoperative infections cause a great deal of suffering for the patient, extend care times and leave a significant economic impact on both the individual and society.
According to national standards in Sweden, the temperature in sterile storage rooms should be within 22±3˚C and the relative humidity 30-70 %. If the humidity exceeds 70%, the risk of microbial growth increases and sterile goods are destroyed by becoming moist and breaking the sterile barrier. It is most sensitive for material packaged in wrapping paper. The function of the wrapping paper is to let in steam during the sterilisation method of steam autoclaving. Steam autoclaving is a very common method for sterilising reusable instruments in surgical units and is performed in most sterile technology units in Sweden. The purpose of the sterilisation process in steam autoclaving is for water vapour to penetrate the wrapping paper. The goods undergo an advanced process involving pressure, heat and saturated steam that leaves a dry and sterile package at the end of the process. If the packaging is not dry or complete, it is not classed as sterile. Due to its ability to let vapour through, the packaging remains sensitive to moisture even during storage. According to standard SIS-TR 57:2020, storages where sterile material is stored must have a controlled environment, which means that the stores should maintain a temperature of 22±3 degrees and a relative humidity (RH%) of 30-70% (unless the manufacturer advises otherwise) and that the colony forming units (cfu) do not exceed 100 cfu/m3.
The background of the study
Operational managers and heads of department in the surgical departments at two hospitals in the south of Sweden reported an unsustainable situation related to high humidity in the hot summer of 2018. For example, sterile packaged goods were found in sterile supplies that were wet and had to be re- sterilised and operations had to be postponed or moved to another room with lower humidity. In September of that year, a project team was set up to review the hospital premises and specify what measures are needed in which premises and what is possible to do to overcome the high humidity. The project group included project managers, property managers, medical technology developers, hygiene nurses, hygiene doctors and representatives from the organization when needed. After 18 months of preliminary work, it was clear that spaces where moisture-sensitive materials are stored should be equipped with a hygrometer. The hygrometer measures the relative humidity in percent (RH %), which means the amount of moisture that the air can contain without being converted into condensation. The hygrometer is connected directly to the maintenance department in one of the hospitals. The department has in turn written a routine for how they should act if they receive an alarm about high RF. There is also a routine written for the units that they are required to follow. This is to get a comprehensive alarm chain when the problems are detected and can thus be addressed in time.
The study setup and aims
The project group concluded that the vast majority of operating theatres will be able to be dehumidified centrally, i.e. the incoming air will be dehumidified. This can be realised because the operating theatres have independent ventilation and because a local dehumidifier is not recommended in operating theatres, which again relates to its impact on the operating room ventilation. In sterile storage rooms, however, central dehumidification is not possible as such a solution would be disproportionately large and costly, which necessitates a local solution for the spaces concerned. So the project group decided to install Dantherm dehumidifiers on the wall of the sterile prosthesis storage room at the surgery in one of the hospitals and in the sterile storage room at the surgery of the other. The sterile storage is larger than the prosthetic storage, so we installed a small CDF 10 condensation dehumidifier in small room and then the bigger room in Varberg required higher dehumidifier capacity and therefore saw the installation of a CDF 40.
The dehumidifiers are synchronised with the hygrometer installed in the same room, enabling the dehumidifier to automatically start and stop as needed. The condensation water is led from the dehumidifier directly to a drain, so no collection vessel needs to be emptied. The air goes through a coarse mesh filter.
For comparison, dehumidifiers from another manufacturer were installed in other sterile rooms of the hospitals.
The aim of the study was to evaluate whether the commercial grade condensation dehumidifiers could contribute to a controlled environment by keeping colony forming units (cfu) in the storage rooms called protesförråd (prostheses storage room) and sterilförråd (sterile storage room) within recommendations of the Swedish Institute of Standards, i.e. 100 cfu/m3 when the dehumidifiers are installed and running.
The CDF’s were connected to the installed hygrometer. The hygrometer is connected to the maintenance department which can monitor that the dehumidifier starts at a pre-set RH % in the room. Technical Service also receives an alarm if the humidity goes up and if the dehumidifier does not start as it is set to do. The dehumidifier is connected to the sewer so it drains the condensation water automatically.
During the data collection period, no special cleaning of the dehumidifiers was carried out. Once they were switched off for the season (around October), they were dismantled and placed in an area with no risk of contamination. Before cleaning, microbiological tests were performed inside the dehumidifiers to check for microorganism contamination. It was highlighted as something very positive that cleaning and maintenance – as well as installation and integration with the BMS system – was all done easily and quickly.
Did it work?
The Dantherm dehumidifier in the prosthesis storage room was initially set to start at 65% RH, however after a while it was discovered that the material stored in the prosthetic store could not withstand RH above 60%. This led the maintenance department staff to adjust the settings so that the Dantherm dehumidifier started at 57% RH. Since the installed humidity sensor has a margin of error of ± 2% RH, it is within the margin of the material's upper limit of 60%. The overall result in the prosthetic store shows that the values have consistently been within acceptable levels of RH % and temperature. Regarding cfu, the values have mostly been well below 100 cfu/m3 except once when the value was 151 cfu/m3, but that was considered an outlier resulting from a defective entry door which could not be closed around the time of the measurement.
In the sterile storage room, the Dantherm dehumidifier was set to be activated at 65% RH. The RH remained within the reference value of 30-70%. Although the registered cfu values are higher than in the prosthesis storage room, they were well below the 100 cfu/m3 limit with just one exception (115 cfu), but that was also considered an outliner resulting from a very high level of staff activity in the room around the time of measurement. Temperatures remained well within acceptable levels.
The conclusion of the study is that both the CDF 10 and CDF 40 contribute to a controlled environment in storage rooms with sterile material. When they were active and operating, they did not contaminate the environment with microorganisms and they were capable of keeping humidity levels, temperature levels well within the set limits. This was in contrast to the dehumidifiers from the other manufacturer which failed to maintain acceptable temperature and humidity levels consistently and therefore they were deemed unfit for purpose by the project group.
As a result of the positive outcome, it was decided to install the Dantherm dehumidifiers in multiple sterile storage rooms.
To learn more about our range of dehumidifiers, and how we can help with commercial building humidity control and climate solutions, get in touch with our team today.
Related products
Featured insights

Regulating humidity levels for pharmaceutical production
The importance of keeping the atmosphere clean

Need help with choosing the right solution? Our team of over 100 climate control experts can assist.
You can also reach out or join the discussion on our Social Media. Check out our LinkedIn page.


